For your birth partner
 ❏ coins for car park/car park payment details
❏ drinks and snacks
❏ phone and charger
❏ camera
❏ books magazine
❏ comfy clothes/shoes/shorts
❏ overnight stay clothes/toiletries etc. if planning/able to stay
❏ coins for car park/car park payment details
❏ drinks and snacks
❏ phone and charger
❏ camera
❏ books magazine
❏ comfy clothes/shoes/shorts
❏ overnight stay clothes/toiletries etc. if planning/able to stay  ❏ coins for car park/car park payment details
❏ drinks and snacks
❏ phone and charger
❏ camera
❏ books magazine
❏ comfy clothes/shoes/shorts
❏ overnight stay clothes/toiletries etc. if planning/able to stay
❏ coins for car park/car park payment details
❏ drinks and snacks
❏ phone and charger
❏ camera
❏ books magazine
❏ comfy clothes/shoes/shorts
❏ overnight stay clothes/toiletries etc. if planning/able to stay  Here is a list of things to consider including in your bag. Even if you are planning a homebirth, it is useful to pack a bag in case your plans change before or during labour:
Here is a list of things to consider including in your bag. Even if you are planning a homebirth, it is useful to pack a bag in case your plans change before or during labour:
 During pregnancy you will have a chance to discuss caring for and feeding your baby, including information about the value of breastfeeding for you and your baby’s health, and how to get breastfeeding off to a good start. It’s never too early to start thinking about how you’re going to feed your baby, but you don’t have to make up your mind until your baby is born. Talking to your midwife about your thoughts and feelings about feeding your baby can be really helpful. You will be supported whatever way you decide to feed your baby.
To help feeding go well, ask your midwife about antenatal breastfeeding classes at your maternity unit or in your local area. This can help you and your partner/supporter to feel more confident and prepared, and help you to avoid some common feeding problems early on. If you have particular questions or concerns about feeding, ask your midwife for an appointment with an infant feeding specialist during pregnancy.
All women are offered the opportunity to hold their baby in skin-to-skin contact straight after birth, for as long as they want. Discuss the benefits of skin-to-skin contact for both you and your baby with your midwife, and how you feel about it.
A midwife will offer to help you to start breastfeeding, or show you how to bottle feed responsively as soon as your baby shows signs that they are ready to feed, usually within the first hour after birth. Your baby won’t be separated from you unless he or she requires special care. After your baby is born you will be offered support from your maternity team to ensure breastfeeding gets off to a positive start. There will also be support available when you are at home.
Explore the related links to find out more about infant feeding.
During pregnancy you will have a chance to discuss caring for and feeding your baby, including information about the value of breastfeeding for you and your baby’s health, and how to get breastfeeding off to a good start. It’s never too early to start thinking about how you’re going to feed your baby, but you don’t have to make up your mind until your baby is born. Talking to your midwife about your thoughts and feelings about feeding your baby can be really helpful. You will be supported whatever way you decide to feed your baby.
To help feeding go well, ask your midwife about antenatal breastfeeding classes at your maternity unit or in your local area. This can help you and your partner/supporter to feel more confident and prepared, and help you to avoid some common feeding problems early on. If you have particular questions or concerns about feeding, ask your midwife for an appointment with an infant feeding specialist during pregnancy.
All women are offered the opportunity to hold their baby in skin-to-skin contact straight after birth, for as long as they want. Discuss the benefits of skin-to-skin contact for both you and your baby with your midwife, and how you feel about it.
A midwife will offer to help you to start breastfeeding, or show you how to bottle feed responsively as soon as your baby shows signs that they are ready to feed, usually within the first hour after birth. Your baby won’t be separated from you unless he or she requires special care. After your baby is born you will be offered support from your maternity team to ensure breastfeeding gets off to a positive start. There will also be support available when you are at home.
Explore the related links to find out more about infant feeding.
 Mothers start to produce colostrum (early breast milk) mid-way through pregnancy. Learning how to express this milk before your baby comes can be very useful, particularly if your baby is likely to be premature or separated from you after birth or if you are diabetic or taking medication for high blood pressure. You can start this from around 37 weeks gestation, and you can collect your colostrum and store it in the freezer if you wish. You may only express a few drops of colostrum when you first start hand expression – this is normal and does not mean that you don’t have any milk. It is still worthwhile practising the technique in preparation for your baby’s arrival.
Read the related links for more information and talk to your midwife or infant feeding specialist.
See How to hand express within Expressing milk in the After your baby is born section for a step by step guide and video.
Mothers start to produce colostrum (early breast milk) mid-way through pregnancy. Learning how to express this milk before your baby comes can be very useful, particularly if your baby is likely to be premature or separated from you after birth or if you are diabetic or taking medication for high blood pressure. You can start this from around 37 weeks gestation, and you can collect your colostrum and store it in the freezer if you wish. You may only express a few drops of colostrum when you first start hand expression – this is normal and does not mean that you don’t have any milk. It is still worthwhile practising the technique in preparation for your baby’s arrival.
Read the related links for more information and talk to your midwife or infant feeding specialist.
See How to hand express within Expressing milk in the After your baby is born section for a step by step guide and video.
 This is a procedure in which a doctor, or specialist midwife attempts to the turn the baby into the correct position using gentle pressure on your abdomen with their hands.
ECV is successful in about 50% of women and is generally safe. One in every 200 babies will need to be delivered by emergency caesarean after an ECV, and your baby will be monitored before and after the procedure to ensure they remain well.
This is a procedure in which a doctor, or specialist midwife attempts to the turn the baby into the correct position using gentle pressure on your abdomen with their hands.
ECV is successful in about 50% of women and is generally safe. One in every 200 babies will need to be delivered by emergency caesarean after an ECV, and your baby will be monitored before and after the procedure to ensure they remain well.
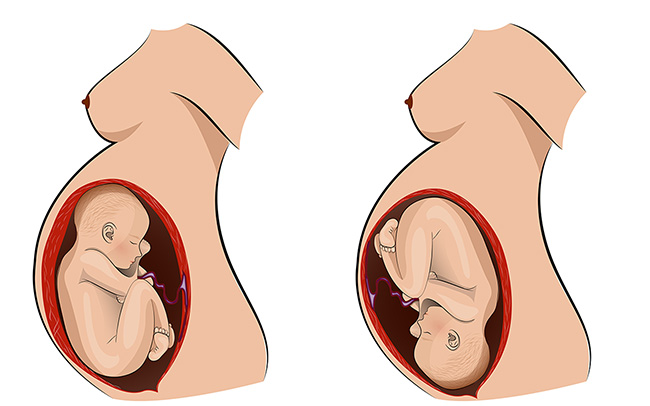
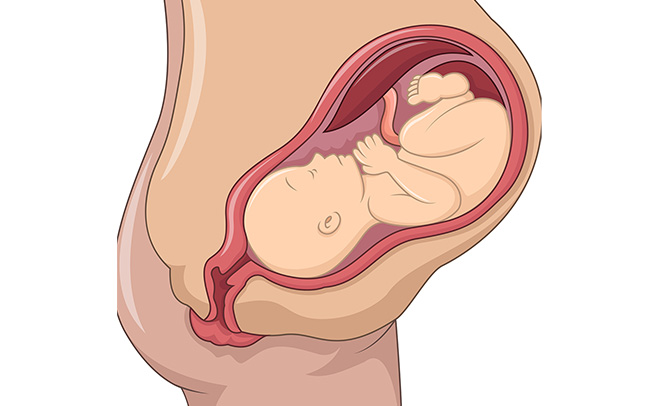 From 36 weeks pregnant, your baby should turn to the head down (cephalic) position in preparation for birth.
A small number of babies will not be in this position, and may be either breech (bottom first) or transverse/oblique (lying sideways across your abdomen). If your midwife suspects that your baby is not in the head down position, you may be offered a scan and appointment with a doctor/specialist midwife to discuss your options. These options can include either attempting to turn your baby (see related links below), vaginal breech birth or planned caesarean birth.
If your baby isn’t head down, don’t worry – there are many options available to you and your team will help you to make any decisions regarding your care moving forward.
From 36 weeks pregnant, your baby should turn to the head down (cephalic) position in preparation for birth.
A small number of babies will not be in this position, and may be either breech (bottom first) or transverse/oblique (lying sideways across your abdomen). If your midwife suspects that your baby is not in the head down position, you may be offered a scan and appointment with a doctor/specialist midwife to discuss your options. These options can include either attempting to turn your baby (see related links below), vaginal breech birth or planned caesarean birth.
If your baby isn’t head down, don’t worry – there are many options available to you and your team will help you to make any decisions regarding your care moving forward.
 When you choose to stop work is a matter of personal preference, but it is worth considering your commute, your working environment, your proximity to your maternity unit and allowing time to prepare for your baby’s arrival. You can discuss this with your midwife or doctor.
Towards the end of pregnancy you may feel quite tired and uncomfortable, and therefore may need help from friends or family to get things done, particularly if you have other children. It’s important to stay active but to also make time for rest, particularly if you aren’t sleeping too well.
When you choose to stop work is a matter of personal preference, but it is worth considering your commute, your working environment, your proximity to your maternity unit and allowing time to prepare for your baby’s arrival. You can discuss this with your midwife or doctor.
Towards the end of pregnancy you may feel quite tired and uncomfortable, and therefore may need help from friends or family to get things done, particularly if you have other children. It’s important to stay active but to also make time for rest, particularly if you aren’t sleeping too well. 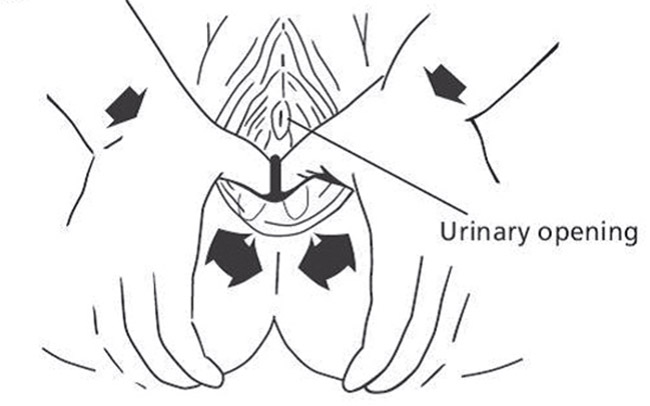 Massaging the perineum (the area between the vagina and anus) in the later weeks of pregnancy has been shown to reduce the likelihood of tearing during birth, and of needing stitches or an episiotomy. You can start this from when you are 34 weeks pregnant and practice it daily/every other day until the birth of your baby.
How to massage your perineum:
Massaging the perineum (the area between the vagina and anus) in the later weeks of pregnancy has been shown to reduce the likelihood of tearing during birth, and of needing stitches or an episiotomy. You can start this from when you are 34 weeks pregnant and practice it daily/every other day until the birth of your baby.
How to massage your perineum:
 Towards the end of pregnancy, you may feel a variety of different emotions as the birth becomes closer. You may feel excited, anxious or even scared – this is all normal. There are things that you can do to help you prepare for birth.
Towards the end of pregnancy, you may feel a variety of different emotions as the birth becomes closer. You may feel excited, anxious or even scared – this is all normal. There are things that you can do to help you prepare for birth.
 Completing a birth preferences plan can help you and your birth partner to think about your choices and preferences during labour and the birth of your baby. During your pregnancy you will have the opportunity to meet with your midwife/doctor and discuss the plan – try and do this around the time of your 34 or 36 week appointment. This will help your team understand the kind of birth you would like.
Read the in app content about labour and birth, then using the birth preferences plan in the Personal care and support plans section write down your thoughts and preferences. See below for what options to consider.
Completing a birth preferences plan can help you and your birth partner to think about your choices and preferences during labour and the birth of your baby. During your pregnancy you will have the opportunity to meet with your midwife/doctor and discuss the plan – try and do this around the time of your 34 or 36 week appointment. This will help your team understand the kind of birth you would like.
Read the in app content about labour and birth, then using the birth preferences plan in the Personal care and support plans section write down your thoughts and preferences. See below for what options to consider.