Female Genital Mutilation (FGM)
What is FGM?
FGM is sometimes called female genital cutting or female circumcision. The definition of Female Genital Mutilation is “any cutting or damage to the external female genitalia that was carried out for non-medical reasons.”
It is a form of child abuse and is a cultural practice that is illegal in the U.K.
FGM is carried out in many parts of the world including Africa, Asia, the Middle East as well as among certain ethnic groups in Central and South America.
Through migration of peoples it is also found in Europe, USA, Canada, Australia and New Zealand.
What are the different types of FGM?
The World Health Organisation (WHO) estimates that 200 million women and girls worldwide have been affected by FGM.
WHO has classified 4 Types of FGM:
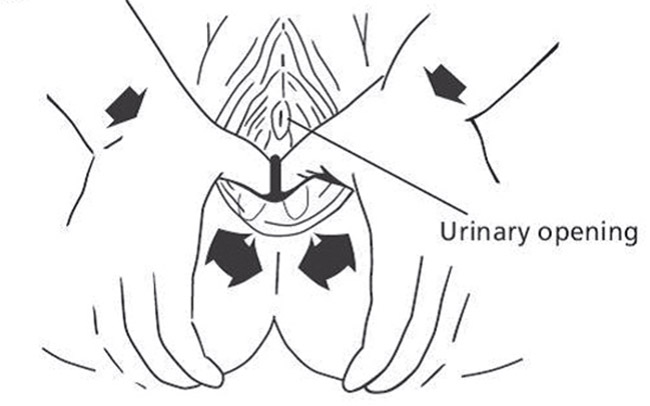
Type 1: part or all of the clitoris and/or clitoral hood has been removed.
Type 2: part or all of the clitoris and/or clitoral hood has been removed, as well as the inner labia (lips that surround and protect the urine hole and vaginal opening).
Type 3 (pharaonic circumcision): the labia or Inner lips have been removed and the remaining edges are then sewn together or fuse together forming a layer of scar tissue with a small single opening at one end.
Type 4: any other harmful practices to a woman’s genitals such as pricking, piercing, stretching or burning.
Possible health problems resulting from FGM
- urinary infections
- vaginal infections
- painful periods
- painful sex
- feeling sad, anxious or depressed
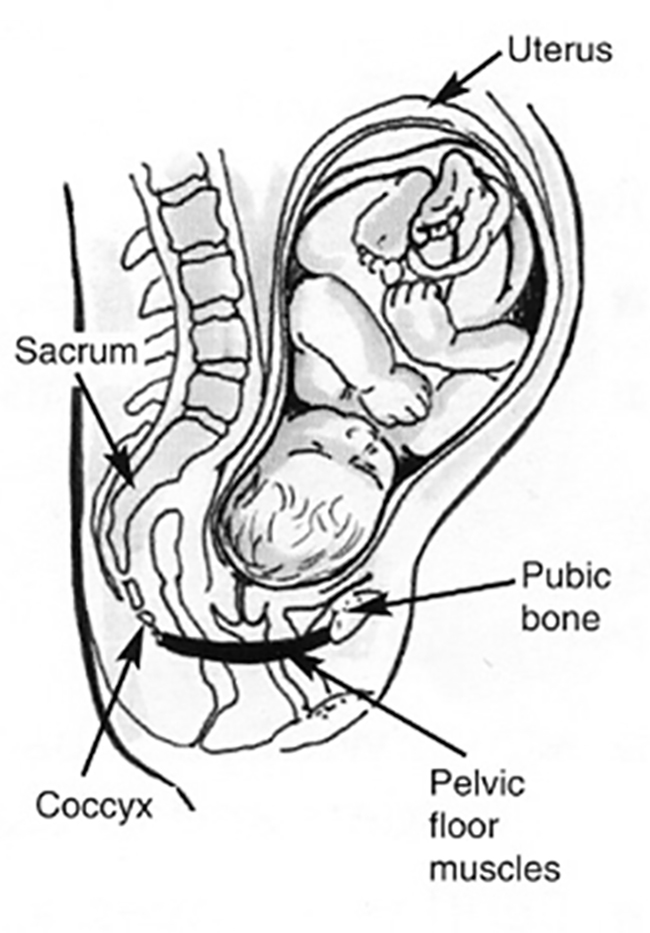
- problems during childbirth.
FGM and pregnancy
In pregnancy all women will be asked about FGM. Women with FGM should have a appointment with a specialist Midwife or Doctor in order to make a personalised plan of care as FGM may have physical and/or psychological consequences that can affect your pregnancy or labour. A safeguarding risk assessment will be carried out to ensure that, if you have a baby girl, she will be protected from FGM.
FGM and UK law
In the UK, it is against the law:
- for anyone to carry out FGM
- to take girls or women who live in the UK to another country to carry out FGM
- to help someone else carry out FGM (this includes making travel arrangements)
- to sew women up after childbirth (known as reinfibulation).
Women with FGM
If you thing you have FGM tell your midwife. She will refer you to a clinic where you will be given support by a FGM specialist midwife.
How can I protect my daughter/s?
The following resources are helpful:
NSPCC/FGM Helpline:
0800 0283550
Police (emergency):
999
Non emergency:
101
Foreign and Commonwealth office (if abroad):
00 44 207 0081500
 Chest pain in pregnancy and/or afer your baby’s birth should never be ignored. Some chest pain can be serious and can lead to a heart attack, heart failure, cardiac arrest or even death. Most women do not suffer from these conditions during or after pregnancy but it is important to recognise the symptoms and, if you have any of them, to seek treatment quickly.
Chest pain in pregnancy and/or afer your baby’s birth should never be ignored. Some chest pain can be serious and can lead to a heart attack, heart failure, cardiac arrest or even death. Most women do not suffer from these conditions during or after pregnancy but it is important to recognise the symptoms and, if you have any of them, to seek treatment quickly.