Reducing the risk of cot death (Sudden Infant Death Syndrome or SIDS)
 Sudden Infant Death Syndrome (SIDS) is the sudden and unexpected death of a baby where no cause is found.
This is rare but it can still happen and there are steps you can take to reduce the risk of this occurring:
Sudden Infant Death Syndrome (SIDS) is the sudden and unexpected death of a baby where no cause is found.
This is rare but it can still happen and there are steps you can take to reduce the risk of this occurring:
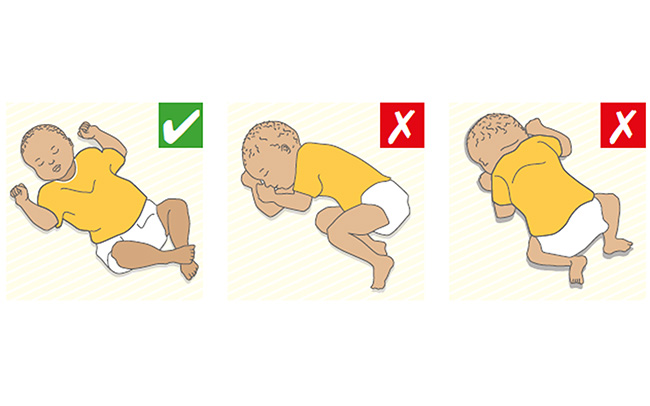
- always place your baby on his/her back to sleep
- babies should not be swaddled when sleeping
- place your baby so his/her feet are right at the end of the cot/moses basket, rather than in the middle, to prevent them from sliding underneath covers
- do not use cot bumpers or quilts, only use sheets and lightweight blankets
- ensure room temperature is between 16-20°C, as overheating your baby can be dangerous
- the safest place for your baby to sleep is in a cot or moses basket in the same room as you, for the first six months.
Safer sleep for babies










