Stillbirth
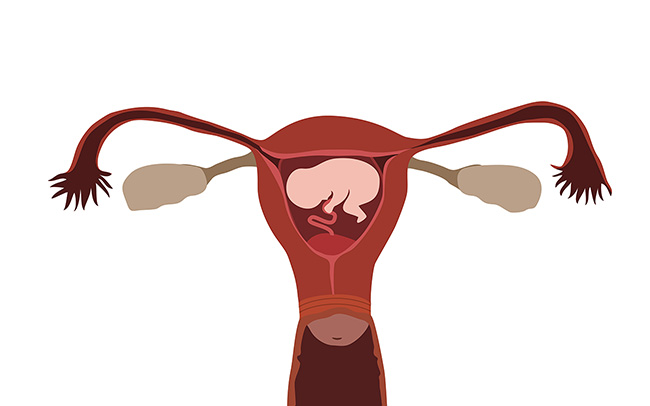
 When a baby passes away after 24 weeks of pregnancy, either before or during birth, this is known as a stillbirth. Stillbirth is one of the most devastating things a family can experience, and a range of support is given through a specialist team (including midwives, obstetricians, counsellors and charities) to parents who are affected by it.
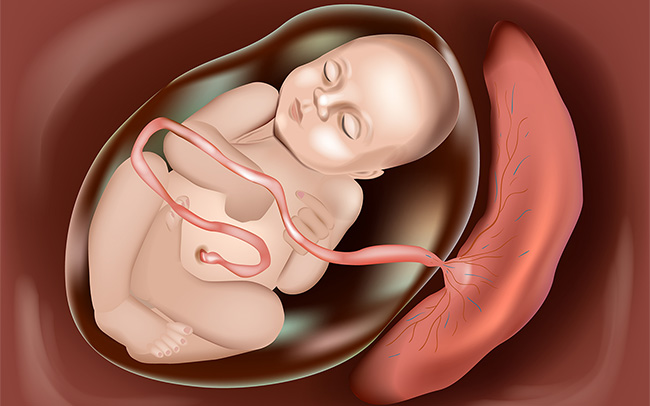
Many stillbirths are linked to a problem with the placenta, which is essential to a baby’s growth and development. If the placenta doesn’t work properly it can cause babies not to receive the oxygen and nutrients they need. Other causes include infection, heavy bleeding (known as haemorrhage), pre-eclampsia and pre-existing diabetes.
Not all stillbirths can be prevented, but there are some simple things that can be done to minimise the risk:
When a baby passes away after 24 weeks of pregnancy, either before or during birth, this is known as a stillbirth. Stillbirth is one of the most devastating things a family can experience, and a range of support is given through a specialist team (including midwives, obstetricians, counsellors and charities) to parents who are affected by it.
Many stillbirths are linked to a problem with the placenta, which is essential to a baby’s growth and development. If the placenta doesn’t work properly it can cause babies not to receive the oxygen and nutrients they need. Other causes include infection, heavy bleeding (known as haemorrhage), pre-eclampsia and pre-existing diabetes.
Not all stillbirths can be prevented, but there are some simple things that can be done to minimise the risk:
- stopping smoking and avoiding alcohol and drugs during pregnancy
- sleeping on your side from around 28 weeks gestation, or turning on to your left side if you wake up on your back overnight
- attending all of your appointments and scans so that your maternity team can monitor your baby’s health
- calling your midwife/going to your maternity unit straight away if your baby’s movements are reduced from what you’re used to feeling.
Portal: Stillbirth